Combined Virna Glaucoma Implant (VGI) Implantation and Pars Plana Vitrectomy for Refractory Aphakic Glaucoma
Poster Presentation - Case Report - Resident
DOI:
https://doi.org/10.35749/7e24y445Keywords:
glaucoma drainage device, pars plana vitrectomy, refractory aphakic glaucomaAbstract
Introduction : Glaucoma drainage devices (GDDs) implantation are frequently indicated for refractory glaucoma. The preferable anterior chamber may be inaccessible for patients with anterior chamber abnormalities.
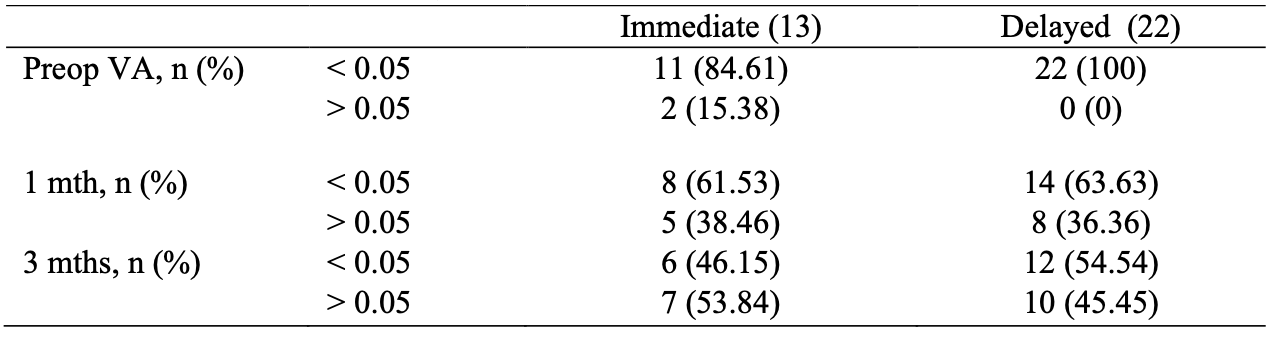
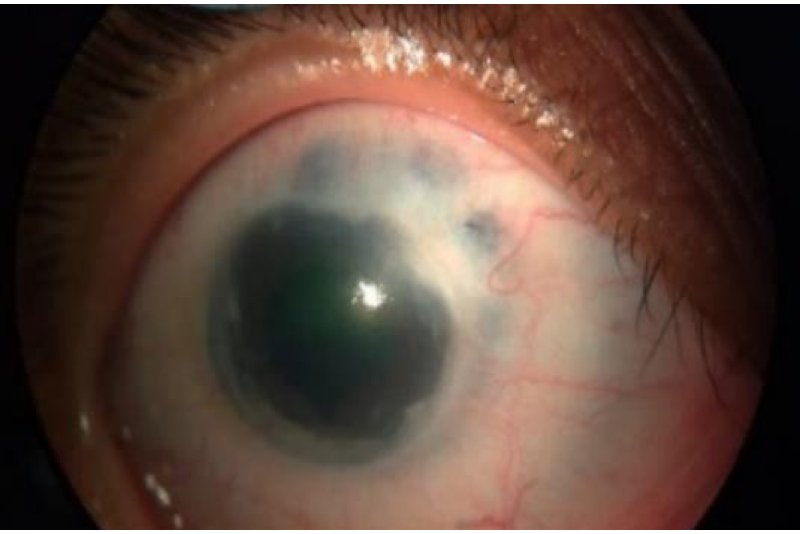
Case Illustration : A 6-year-old boy presented with high intraocular pressure (IOP) on the right eye (RE) four months before admission. Cataract surgery on both eye was done four years prior, due to congenital cataract. On examination, the visual acuity of the RE was hand movement with IOP 61mmHg with medications. Anterior chamber was shallow, posterior synechiae was found and posterior segment was hard to be evaluated. The fellow eye was nonfunctional with IOP 31mmHg. Pars plana vitrectomy (PPV) was performed followed by implantation of GDD (Virna Glaucoma Implant) with posterior chamber sulcus tube placement without adding a new incision. Post-operatively, IOP was 3mmHg and choroidal detachment was found. With steroid medication, satisfactory IOP control was achieved within three weeks of follow-up. Visual acuity of RE was improved to 0.5/60.
Discussion : In eyes with shallow anterior segments, tube placed in the anterior chamber may increase the risk of corneal endothelial injury. Placement of the silicone tube in the posterior chamber sulcus is an effective alternative technique. Although it is relatively safe in experienced hands, vitrectomy and insertion of the tube into the posterior segment carries significant risks, including choroidal detachment. Careful monitoring and management is needed to control IOP and maintain vision.
Conclusion : Combined GDD implantation and PPV may be considered for refractory aphakic glaucoma, showing favorable outcomes with a relatively safe procedure.
Downloads
References
(-)
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.