The Visual Rehabilitation of Bilateral Posterior Lens Luxation In Children: A Case Report
DOI:
https://doi.org/10.35749/journal.v48i2.100668Keywords:
luxated, visual rehabilitation, aphakic spectacles, lensectomyAbstract
Introduction: Dislocated lens can be subluxated (partial) or luxated (complete), which can cause visual impairment in children. Conservative visual rehabilitation is an option for luxated lens treatment.
Purpose: This study reports the possibility for visual rehabilitation of bilateral of bilateral luxated lens in children.
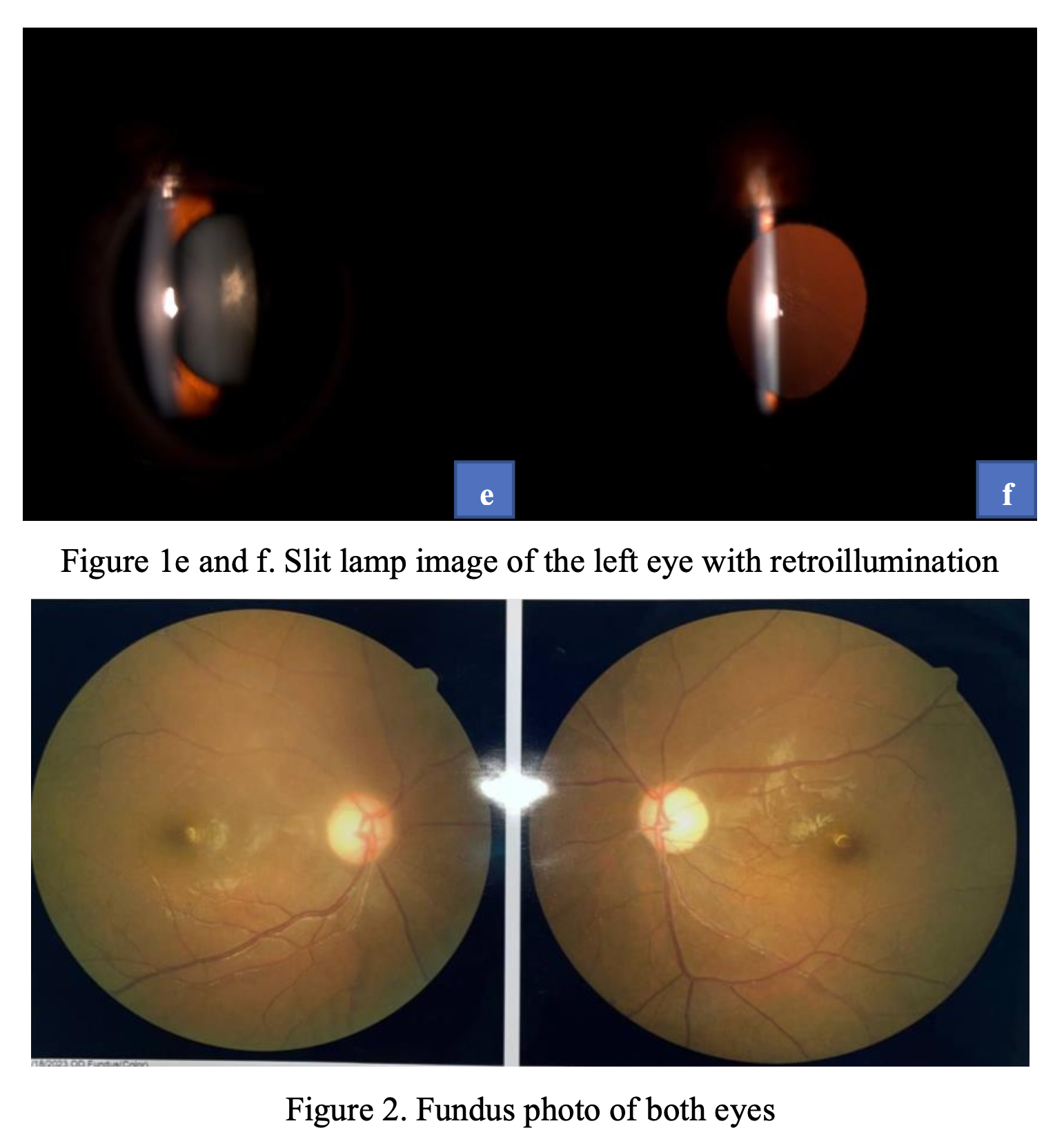
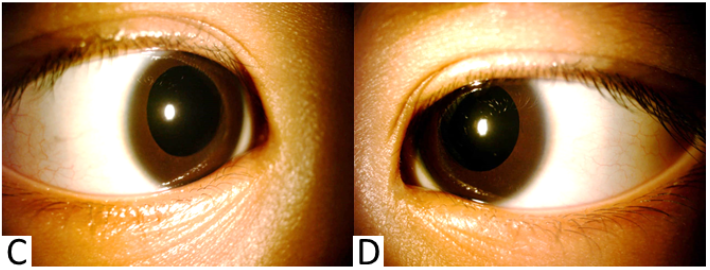
Case Report: A 3-year-old boy came to the outpatient clinic of Dr. Saiful Anwar General Hospital with complaints of blurred vision on both eyes. The child would always bring objects close to his eyes since the past year. There was no history of ocular injury nor development disorder. Uncorrected visual acuities with LEA symbol on both right and left eyes were 6/114. The best-corrected visual acuity (BCVA) of the right eye was 6/45 and left eye was 6/9 with both S+11.00. Iridodonesis and aphakic lenses were found during slit-lamp examination of both eyes. The intraocular pressures were 14.2 mmHg on the right eye and 17.3 mmHg on the left eye. The lenses were seen in the vitreous cavities during funduscopy and ultrasonography examination. After 1 month of using spectacles, the BCVA of the right eye was 6/18 and that of the left eye was 6/18 with the binocular BCVA was 6/15. Lensectomy with pars plana vitrectomy was planned to prevent complication.
Conclusion: Conservative visual rehabilitation is important to prevent amblyopia in children with luxated lenses and surgical treatment is needed to prevent complication. In this patient, aphakic spectacles were given for visual rehabilitation pending operative treatment.
Downloads
References
Qayyum S, Chaudhary A, Hussain M, Mushtaq A, Sharif S, Dogar ZJPJoO. Ectopia Lentis Etiology and Management in Children. 2016;32(3).
Simon MA, Origlieri CA, Dinallo AM, Forbes BJ, Wagner RS, Guo SJJopo, et al. New management strategies for ectopia lentis. 2015;52(5):269-81.
Liu Y, Chen W. Pediatric lens diseases: Springer; 2017.
Jin G-M, Fan M, Cao Q-Z, Lin J-X, Zhang Y-C, Lin J-Q, et al. Trends and characteristics of congenital
ectopia lentis in China. 2018;11(9):1545.
Meester JA, Verstraeten A, Schepers D, Alaerts M, Van Laer L, Loeys BLJAocs. Differences in
manifestations of Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome. 2017;6(6):582.
Shafique M, Muzaffar W, Ishaq MJIo. The eye as a window to a rare disease: ectopia lentis and
homocystinuria, a Pakistani perspective. 2016;36(1):79-83.
Dietz H. Marfan syndrome. GeneReviews®[Internet]: University of Washington, Seattle; 2017.
Karoulias SZ, Beyens A, Balic Z, Symoens S, Vandersteen A, Rideout AL, et al. A novel ADAMTS17
variant that causes Weill-Marchesani syndrome 4 alters fibrillin-1 and collagen type I deposition in the extracellular matrix. 2020;88:1-18.
Shah MH, Bhat V, Shetty JS, Kumar AJMv. Whole exome sequencing identifies a novel splice-site
mutation in ADAMTS17 in an Indian family with Weill-Marchesani syndrome. 2014;20:790.
Acucella G, Finale E, Auletta G, Guala AJAJoMCR. Isolated Dislocation of Ocular Lens. 2016;4(3):97-100.
Yang Y, Zhou Y-l, Yao T-t, Pan H, Gu P, Wang Z-yJBJoO. Novel p. G1344E mutation in FBN1 is
associated with ectopia lentis. 2020.
Reinstein E, Smirin-Yosef P, Lagovsky I, Davidov B, Amit GP, Neumann D, et al. A founder mutation in ADAMTSL4 causes early-onset bilateral ectopia lentis among Jews of Bukharian origin. 2016;117(1):38-41.
van Bysterveldt KA, Al Taie R, Ikink W, Oliver VF, Vincent ALJOG. ADAMTSL4 assessment in ectopia lentis reveals a recurrent founder mutation in Polynesians. 2017;38(6):537-43.
Deng D, Li J, Yu M. Postoperative Visual Rehabilitation in Children with Lens Diseases. Pediatric Lens Diseases: Springer; 2017. p. 353-69.
Leuder G, Archer S, Hered RW, Karr DJ, Kodsi SR, Kraft SP, et al. Basic and Clinical Science Course, Section 6: Pediatric Ophthalmology and Strabismus. 2019.
Baradaran-Rafii A, Shirzadeh E, Eslani M, Akbari MJJoo, research v. Optical correction of aphakia in children. 2014;9(1):71.
Repka MX. Visual rehabilitation in pediatric aphakia. Pediatric Cataract. 57: Karger Publishers; 2016. p.49-68.
Tromans C, Wilson H. The Refractive Management of Infantile Aphakia and Pseudophakia. Congenital Cataract: Springer; 2017. p. 165-72.
Lambert SR, Kraker RT, Pineles SL, Hutchinson AK, Wilson LB, Galvin JA, et al. Contact lens correction of aphakia in children: a report by the American Academy of Ophthalmology. 2018;125(9):1452-8.
Peyman GA. Vitreoretinal surgical techniques: Routledge; 2019.
Singh R, Kumari N, Katoch D, Sanghi G, Gupta A, Dogra MRJJopo, et al. Outcome of 23-gauge pars plana vitrectomy for pediatric vitreoretinal conditions. 2013;51(1):27-31.
Babu N, Muraly P, Ramasamy KJR. Twenty-three-gauge two-port pars plana lensectomy for the management of ectopia lentis in children. 2010;30(6):971-4.
Manning S, Lanigan B, O'Keefe MJJoAAfPO, Strabismus. Outcomes after lensectomy for children with Marfan syndrome. 2016;20(3):247-51.
Fiorentzis M, Viestenz A, Heichel J, Seitz B, Hammer T, Viestenz AJCA. Methods of fixation of intraocular lenses according to the anatomical structures in trauma eyes. 2018;31(1):6-15.
Pirouzian A, Ip KCJJoC, Surgery R. Anterior chamber phakic intraocular lens implantation in children to treat severe anisometropic myopia and amblyopia: 3-year clinical results. 2010;36(9):1486-93.
Brandner M, Thaler-Saliba S, Plainer S, Vidic B, El-Shabrawi Y, Ardjomand NJPO. Retropupillary fixation of iris-claw intraocular lens for aphakic eyes in children. 2015;10(6):e0126614.
Asadi R, Kheirkhah AJO. Long-term results of scleral fixation of posterior chamber intraocular lenses in children. 2008;115(1):67-72. e1.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2022 Yunneke Renna Xaverina, Anny Sulistiyowati, Lely Retno Wulandari

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.