Horner Syndrome Related to Nasopharyngeal Carcinoma
DOI:
https://doi.org/10.35749/journal.v41i2.22Abstract
Background: Horner syndrome classically presents with ipsilateral blepharoptosis, pupillary miosis, and facial anhidrosis. The syndrome results from interuption of the sympathetic innervation to the eye and ocular adnexae.
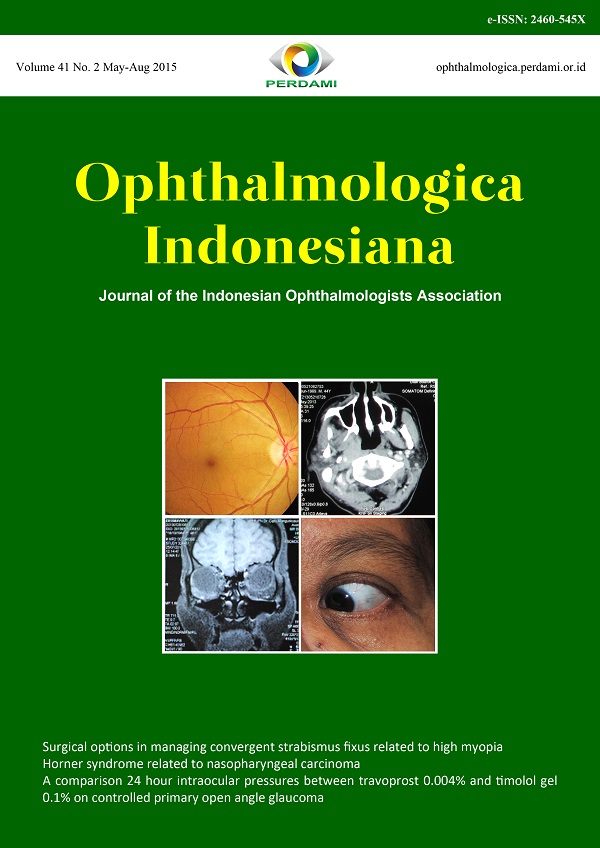
Case Illustration: A 43-year-old male complaining of drop of upper eyelid right eye, anhidrosis right side of face, and numbness on his right face since 7 months previously. He had painless, slowly enlarging, right-sided neck mass that was first noticed approximately 7 months before presentation. The biopsy and CT scan confirmed nasopharyngeal carcinoma (NPC). Best corrected visual acuity of both eyes was 6/6, normal IOP and ocular movement. There was mild ptotic eyelid 2 mm of his right eye. Both anterior segment within normal limit. There was unequal pupils greater in the dark, with pupil size of the right eye 3 mm and left eye 5 mm. The pupils were reactive to light, without afferent pupillary defect. Both posterior segment examination were unremarkable. There was reduced sensibility of the right face at maxila and mandibular region. The patient was diagnosed with Horner syndrome with involvement of right trigeminal nerve at maxillary and mandibular division, and involvement of sweat glands corellate with preganglionic lesion.
Conclusion: Nasopharyngeal carcinoma that affects oculosympathetic pathway may give clinical signs as Horner syndrome. There was found involved of sweat gland in this case, it is correlated with lesion in preganglionic. But the anhidrosis occurs only in maxila and mandibular region, therefore post ganglionic involvement can not be ruled out.
Keywords: Horner syndrome, nasopharyngeal carcinoma
Downloads
References
Kawasaki A. Disorders of pupillary function, accommodation, and lacrimation. In: Miller NR, Newman NJ, editors. Walsh & Hoyt’s Clinical Neuro-Ophthalmology. 6th Edition. Philadelphia: Lippincott Williams & Wilkins; 2005. P. 749-58.
George A, Haydar AA, Adams WM. Imaging of horner’s syndrome. Clinical Radiology. 2008;63:499-505.
Liu GT, Volpe NJ, Galetta SL. Neuro-ophthalmology: diagnosis and management. 2nd ed. Philadelphia: Saunders Elsevier; 2010. P. 428-41.
Politi M, Toro C, Cian R, Costa F, Robiony M. Hornes’s syndrome due to a large schwannoma of the cervical sympathetic chain: report of case. J Oral Maxillofac Surg. 2005;63:707-10.
Lee AG, Brazis PW. Clinical pathway in neuro-ophthalmology. New York: Thieme Medical Publisher Inc; 2003. P. 445-56.
American Academy of Ophthalmology Staff. Neuro-ophthalmology. Section 5. San Francisco: American Academy of Ophthalmology; 2011-2012. P. 266-8.
Ropper AH, Brown RH. Adam and victor’s principles of neurology. New York: McGraw-Hill Companies; 2008. P. 242-3.
Agarwal A, Agarwal A. Manual of Neuro-ophthalmology. New Delhi: Jaypee Brothers Medical Publishers; 2009. P.66-70.
Koc F, Kavuncu S, Kansu T, Acaroglu G, Firat E. The sensitivity and specificity of 0,5% apraclonidine in the diagnosis of oculosympathetic paresis. Br J Ophthalmol. 2005;89:1442-4.
Chen P, Hsiao C, Chen J, Lu D, Chen W. Efficacy of apraclonidine 0.5% in the diagnosis of horner syndrome in pediatric patient under low or
high illumination. Am J ophthalmol. 2006;142:469-74.
Kidd DP, Newman NJ, Biousse V. Neuro-ophthalmology. Philadelphia: Saunders Elsevier; 2008. P. 270.
Nambiar S, Blain F, Agrawal P, Shad A, Ahluwalia A. Isolated postganglionic horner syndrome some lesson learned. Can J Ophthalmol. 2012;47:e26-7.
Kim JD, Hashemi N, Gelman R, Lee AG. Neuroimaging in ophthalmology. Saudi Journal of Ophthalmology. 2012;26:401-7.
Frishberg B. Miscellaneous tumors of neuro-ophthalmologic interest. In: Miller NR, Newman NJ, editors. Walsh & Hoyt’s Clinical Neuro-Ophthalmology. 6th Edition. Philadelphia: Lippincott Williams & Wilkins; 2005. P. 1684-6.
Wilhelm A, Wilhelm B. Diagnosis of pupillary disorders. In: Schiefer U, Wilhelm A, Hart A, editors. Clinical neuro-ophthalmology. New York: Springer; 2007. P. 63.
Crippa SV, Borruat FX, Kawasaki A. Pupillary dilation lag is intermittently present in patients with a stable oculosympathetic defect (horner syndrome). Am J Ophthamol. 2007;143:712-5.
Ahmed R, Biousse V, Bruce BB, Chan SS, Clark D, Cockerham KP, et al. Neuro-ophthalmology. In: Evans RW, editor. Neurologic clinics. Philadelphia: Saunders Elsevier; 2010. P. 667-72.
Fetzer SJ. Clinical insight and review: recognizing horner’s syndrome. Journal of Perianesthesia Nursing:15:124-8.
Jacobson DM, Berg R, Grinstead GF, Kruse JR. Duration of positive urine for cocaine metabolite after ophthalmic administration; implications for testing patients with suspected horner syndrome using ophthalmic cocain. Am J Ophthalmol. 2001;131:742-7.
Watts P, Satterfield D, Lim MK. Adverse effects of apraclonidine used in the diagnosis of horner syndrome in infants. J AAOPS. 2007;11:282-3.
Freedman KA, Brown SM. Topical apraclonidine in the diagnosis of suspected horner syndrome. J neuroophthalmol. 2005;25:83-5.
Morales J, Brown SM, Abdul AS, Crosson CE. Ocular effects of apraclonidine in horner syndrome. Arhc Ophthalmol. 2000;118:951-4.