REFRACTIVE OUTCOMES COMPARISON IN LIMBAL RELAXING INCISION BASED ON INCISION DEPTH IN MANAGING CORNEAL ASTIGMATISM DURING CATARACT SURGERY
Oral Presentation - Experimental Study - General practitioner
DOI:
https://doi.org/10.35749/ebawbr98Keywords:
limbal relaxing incision, corneal astigmatism, cataract surgeryAbstract
Abstract
Introduction & Objectives : Introduction: Prevalence of clinically significant astigmatism of more than 1D can be found in 20 to 50% population those undergo cataract surgery. During phacoemulsification surgery, astigmatism could be corrected by toric intraocular lens (IOL) or incisional technique such as limbal relaxing incision (LRI). LRI are safe and inexpensive procedures thus results in satisfying outcomes with surgeon’s precise phacoemulsification incision and accurate LRI arc position, which most appropriate treatment choice for surgeons in rural area that has problematic access towards IOL supply. Objectives: To compare refractive outcomes of LRI technique with incision depth of 500um and 600um using diamond knife corresponding with phacoemulsification cataract removal.
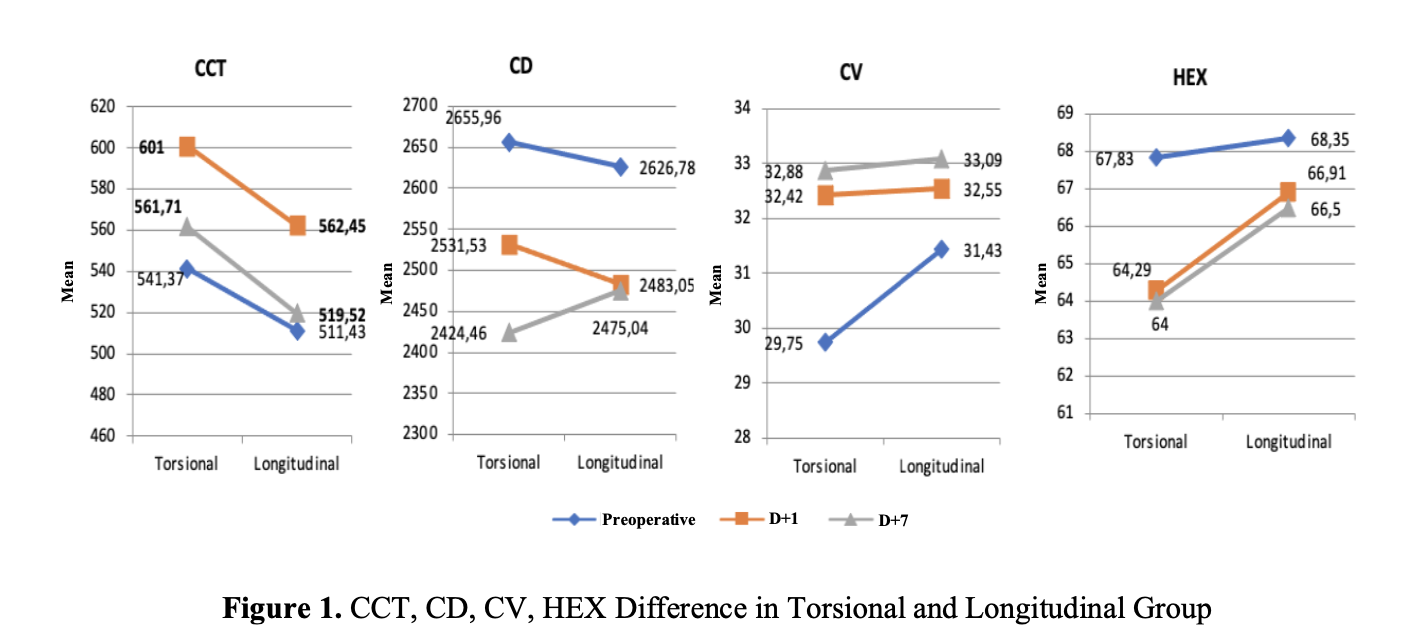
Methods : Prospective cumulative interventional case study included 30 eyes of consecutive cataract corneal astigmatic patients power >1.0D those undergoing LRI and phacoemulsification. Length, numbers, and arc position of LRI were calculated on LRI Calc application to obtain best results in minimal astigmatism residual. Uncorrected visual acuity, intraocular pressure, and keratometric cylinder were also analysed before surgery, Day-1, Day-7, and 1-Month post-operation.
Results : Day-1 follow-up keratometry shown that corneal astigmatism was still fluctuated, day-7 follow-up was even better with significant improvement in visual acuity. 1-Month post-operation has reached target correction. Moreover, visual acuity and residual astigmatism was better in 600um incision depth.
Conclusion : When toric IOLs are not available or contraindicated, LRI could be a good option in correcting astigmatism with better refractive outcomes trend in 600um incision depth. LRI results better be evaluated in day-7 and 1-Month post-LRI, which may due to more stable corneal surface.
Downloads
References
(-)
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.