UNVEILING OPHTHALMOLOGICAL FINDINGS IN CORNELIA DE LANGE SYNDROME: A RARE CASE REPORT
DOI:
https://doi.org/10.35749/cbyqa786Keywords:
Cornelia de Lange syndrome, ptosis, high myopia, cataractAbstract
Introduction: Cornelia de Lange syndrome (CdLS) is a rare congenital disorder with a distinctive combination of physical, cognitive, and behavioral features. This syndrome impacts multiple systems in the body, including the eyes.
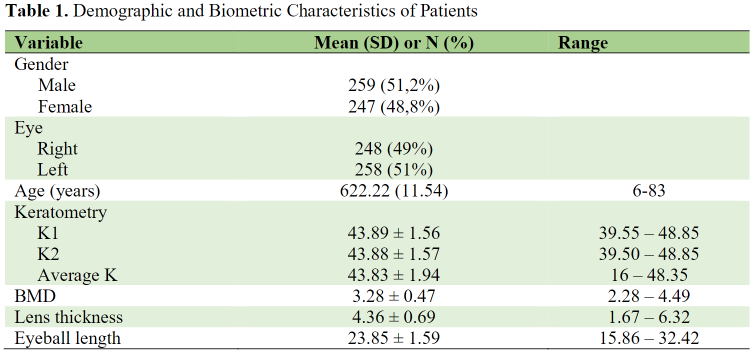
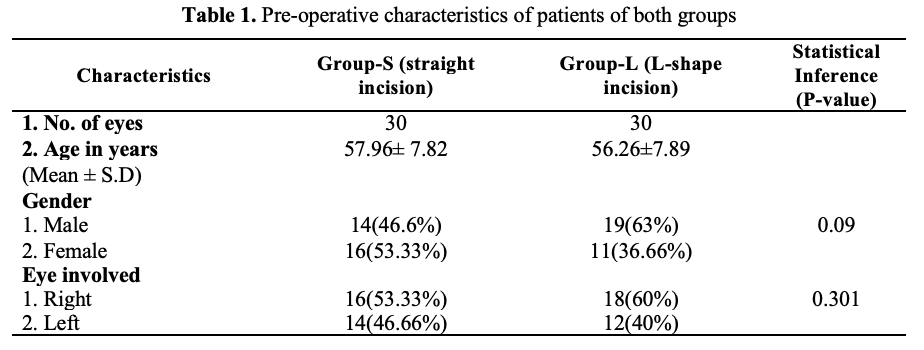
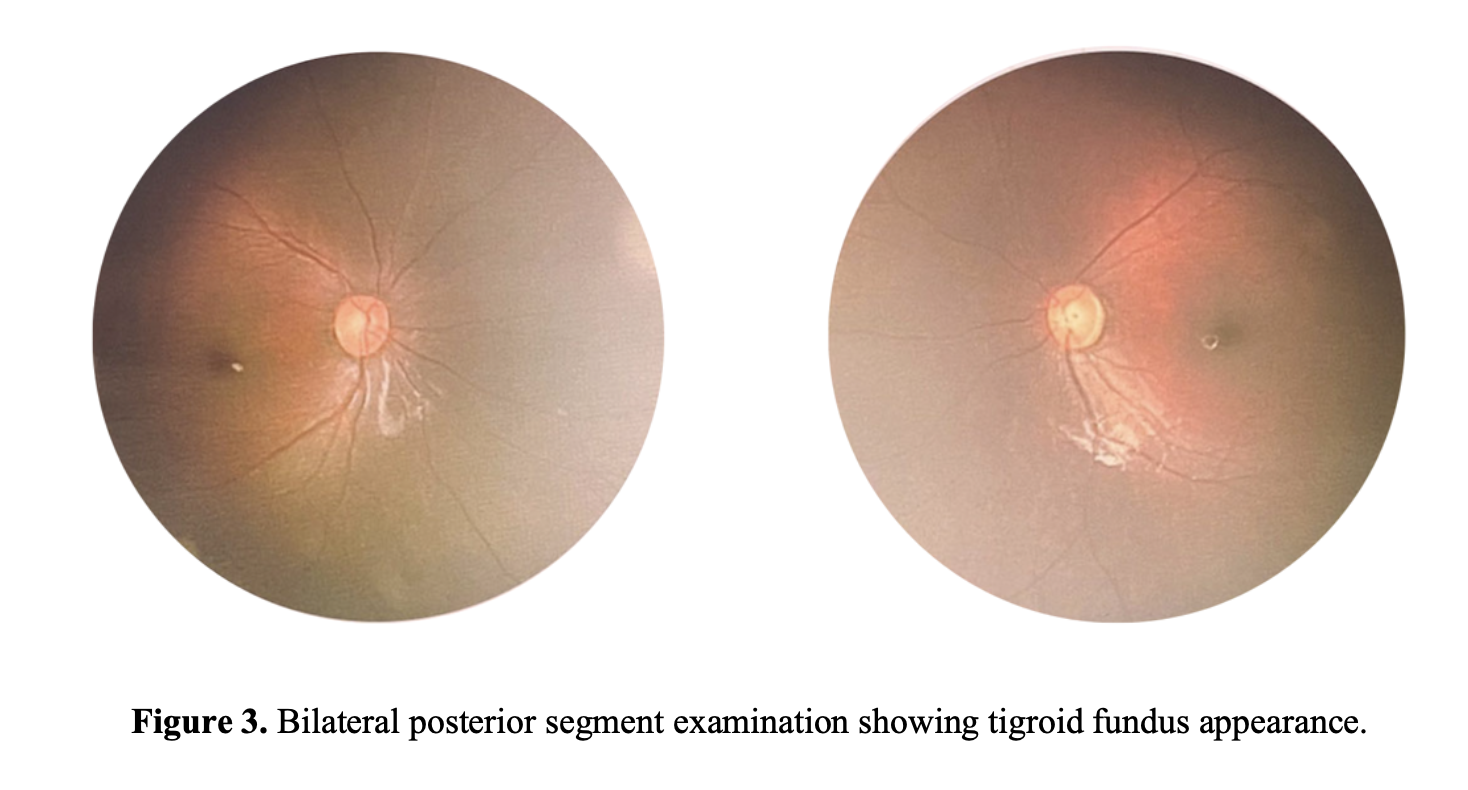
Case Report: A three-year-old boy with classic CdLS, emphasizing the ophthalmological findings of left eye ptosis, high myopia and astigmatism, microcornea, bilateral “dot opacities” cataracts, and tigroid fundus appearance. The patient was prescribed corrective eyeglasses to prevent amblyopia.
Discussion: The clinical scoring system devised by the International CdLS Consensus Group aids in classifying CdLS cases into classic and non-classic variants, as well as guiding clinical genetic testing decisions. In all instances of suspected or confirmed CdLS, it is imperative that an ophthalmologist performs an initial eye examination promptly. Therefore, acquiring familiarity with the potential ophthalmological findings of CdLS is crucial. Common ocular presentations encompass features such as synophrys, thick eyebrows, long eyelashes, ptosis, myopia, microcornea, nasolacrimal duct obstruction, peripapillary pigment ring, and blepharitis. Meanwhile, less frequently encountered ocular manifestations include hyperopia and astigmatism, cataracts, microphalmia, glaucoma, optic nerve pallor and hypoplasia, nystagmus, and strabismus.
Conclusion: Timely diagnosis, precise interventions, and regular ophthalmological monitoring are pivotal in preventing complications and enhancing visual function, thus improving the quality of life of individuals with CdLS.
Downloads
References
Kline AD, Moss JF, Selicorni A, Bisgaard AM, Deardorff MA, Gillett PM, et al. Diagnosis and management of Cornelia de Lange syndrome: first international consensus statement. Nat Rev Genet. 2018; 19:649–66.
Kline AD, Grados M, Sponseller P, Levy HP, Blagowidow N, Schoedel C, et al. Natural history of aging in Cornelia de Lange syndrome. Am J Med Genet C Semin Med Genet. 2007;145C:248–60.
Shi A, Levin AV. Ophthalmologic findings in the Cornelia de Lange syndrome. Ophthalmic Genet. 2019; 40:1–6.
Huisman SA, Redeker EJW, Maas SM, Mannens MM, Hennekam RCM. High rate of mosaicism in individuals with Cornelia de Lange syndrome. J Med Genet. 2013; 50:339–44.
Nallasamy S, Kherani F, Yaeger D, McCallum J, Kaur M, Devoto M, et al. Ophthalmologic findings in Cornelia de Lange Syndrome: a genotype-phenotype correlation study. Arch Ophthal. 2006; 124:552–7.
Boyle MI, Jespersgaard C, Brøndum-Nielsen K, Bisgaard AM, Tümer Z. Cornelia de Lange syndrome. Clin Genet. 2015; 88:1–12.
Wygnanski-Jaffe T, Shin J, Perruzza E, Abdolell M, Jackson LG, Levin AV. Ophthalmologic findings in the Cornelia de Lange syndrome. J AAPOS. 2005; 9:407–15.
Levin A V., Seidman DJ, Nelson LB, Jackson LG. Ophthalmologic findings in the Cornelia de Lange syndrome. J Pediatr Ophthalmol Strabismus. 1990; 27:94–102.
Kim IT, Park JW, Choi WC. A Korean case of Cornelia de Lange syndrome. Korean J Ophthalmol. 2005; 19:153–5.
American Academy of Ophthalmology. Pediatric Ophthalmology and Strabismus. In: Khan A, Chang TCP, El-Dairi MA, Lee KA, Utz VM, Mireskandari K, et al., editors. 2022-2023 Basic and Clinical Science Course. American Academy of Ophthalmology; 2022.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Dian Estu Yulia, Sabrina Tan

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.