AN OVERVIEW OF REFRACTIVE ERRORS AMONG CHILDREN IN KOTA SOE DISTRICT, INDONESIA
DOI:
https://doi.org/10.35749/journal.v49i2.100724Keywords:
Refractive error, myopia, screen time, outdoor timeAbstract
Introduction: Refractive error is one of the most common preventable causes of blindness in the world. Screen time and outdoor time are known as risk factors for its prevention. This study aims is to show the prevalence of children's refractive error and the difference between screen time and outdoor time.
Methods: This study used a cross-sectional design to examine children's refractive error from 10 to 14 years old at five child development centers located across SoE from March 2020 to August 2021. Screen time and outdoor time data were obtained using a questionnaire, grouped into low-medium and high groups, and analyzed the differences between groups.
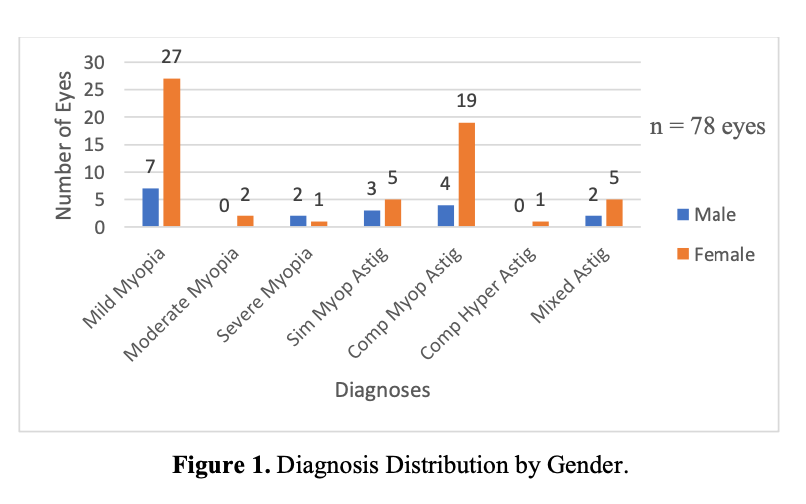
Result: In this study, there are 429 participants with an average age of 12.65 ± 1.44 years old. The prevalence of refractive error is 9.56% and the most common error is mild myopia (43.59%). Refractive error in females is more common than in males (75.61%) and distributed in all age groups. There is no significant difference between refractive error prevalence and the amount of screen time (t 0.500; p: 0.480) and outdoor time (t: 0.944; p: 0.331).
Conclusion: The most common refractive error in this study is mild myopia. There is no refractive error prevalence difference in screen time and outdoor time.
Downloads
References
Tortora GJ, Derrickson B. The Special Senses. In: Roesch B, editor. Principles of Anatomy and Physiology. 12th ed. United States of America: John Wiley & Sons, Inc; 2009. p. 604–5.
Remington LA, Falk K. Clinical Anatomy and Physiology of the Visual System. 3rd ed. Missouri: Elsevier Butterworth-Heinemann; 2012.
Bourne RRA, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, et al. Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Heal. 2013;1.
Chuck RS, Jacobs DS, Lee JK, Afshari NA, Vitale S, Shen TT, et al. Refractive Errors & Refractive Surgery Preferred Practice Pattern. American Academy of Ophthalmology; 2017.
Verhoeven VJM, Cumberland P, Bertelsen G, Wolfram C, Buitendijk GHS, Albert Hofman Johannes R. Vingerling, Robert W. A. M. Kuijpers, René Höhn, Alireza Mirshahi, Anthony P. Khawaja, Robert N. Luben, Maja Gran Erke, Therese von Hanno, Omar Mahroo, Ruth Hogg, Christian Gieger, Audrey Cougnard-Grégoire, Eleftherios Anastasop CM van D. Prevalence of refractive error in Europe: the European Eye Epidemiology (E3) Consortium. Eur J Epidemiol. 2015;30:305–15.
Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ [Internet]. 2008;86(1):1–80. Available from: https://www.who.int/bulletin/volumes/86/1/07-041210/en/
Lou L, Yao C, Jin Y, Perez V, Ye J. Global Patterns in Health Burden of Uncorrected Refractive Error. Invest Ophthalmol Vis Sci. 2016;57:6271–7.
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;124(3):e24–5.
Gomez-Salazar F, Campos-Romero A, Gomez-Campaña H, Cruz-Zamudio C, Chaidez-Felix M, Leon-Sicairos N, et al. Refractive errors among children, adolescents and adults attending eye clinics in Mexico. Int J Ophthalmol. 2017;10(5):796–802.
Halim A, Suganda R, Sirait SN, Memed FK, Syumarti, Rini M, et al. Prevalence and associated factors of uncorrected refractive errors among school children in suburban areas in Bandung, Indonesia. Cogent Med. 2020;7:1–13.
Harb EN, Wildsoet CF. Origins of Refractive Errors: Environmental and Genetic Factors. Annu Rev Vis Sci. 2019;5(1):47–72.
Enthoven CA, Willem L. Tideman, Jan Roelof Polling, Junwen Yang-Huang, Klavera HRCCW. Smarphone use associated with refractive error in teenagers: The myopia app study. Ophthalmology. 2021;1–8.
Alvarez-Peregrina C, Sánchez-Tena MÁ, Martinez-Perez C, Villa-Collar C. The Relationship Between Screen and Outdoor TIme With Rates of Myopia in Spanish Children. Front Public Heal. 2020;8.
Ryan T. Sample Size Determination and Power. John Wiley and Sons; 2013.
Badan Pusat Statistik. Jumlah Penduduk Per Kelompok Umur di Kecamatan Kota SoE Tahun 2019. Timor Tengah Selatan: Badan Pusat Statistik; 2019.
Nikmah ST, Rifada RM, Santoso PTR. Refractive Errors in State Junior High School Students in Bandung. Althea Med J. 2016;3(4):545–8.
Tang Y, Chen A, Zou M, Liu Z, Young CA, Zheng D, et al. Prevalence and time trends of refractive error in Chinese children: A systematic review and meta-analysis. J Glob Health. 2021;11(08006).
Murthy GVS, Gupta SK, Ellwein LB, Muñoz SR, Pokharel GP, Sanga L, et al. Refractive Error in Children in an Urban Population in New Delhi. Invest Ophthalmol Vis Sci [Internet]. 2002;43(3):623–31. Available from: https://iovs.arvojournals.org/article.aspx?articleid=2200126
Lu B, Congdon N, Liu X, Choi K, Lam DSC, Zhang M, et al. Associations Between Near Work, Outdoor Activity, and Myopia Among Adolescent Students in Rural ChinaThe Xichang Pediatric Refractive Error Study Report No. 2. Arch Ophtalmol. 2009;127(6):769–75.
Jones-Jordan LA, Sinnott LT, Chu RH, Cotter SA, Kleinstein RN, Manny RE, et al. Myopia Progression as a Function of Sex, Age, and Ethnicity. Clin Epidemiol Res. 2021;62(10):36.
Tricard D, Marillet S, Ingrand P, Bullimore MA, Bourne RRA, Leveziel N. Progression of myopia in children and teenagers: a nationwide longitudinal study. Br J Ophthalmol [Internet]. 2022;106(8):1104–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9340031/
Yam JC, Tang SM, Kam KW, Chen LJ, Yu M, Law AK, et al. High prevalence of myopia in children and their parents in Hong Kong Chinese Population: the Hong Kong Children Eye Study. Acta Ophthalmol. 2020;98(5):e639–48.
Sheeladevi S, Seelam B, Nukella PB, Modi A, Ali R, Keay L. Prevalence of refractive errors in children in India: a systematic review. Clin Exp Optom. 2018;101(4):495–503.
Walline JJ, Lindsley KB, Vedula SS, Cotter SA, Mutti DO, Ng SM, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020;
Li T, Zhou X, Chen X, Qi H, Gao Q. Refractive Error in Chinese Preschool Children: The Shanghai Study. Eye Contact Lens. 2019;45(3):182–7.
Liang Y, Leung T-W, Lian JT, Kee C-S. Significant increase in astigmatism in children after study at home during the COVID-19 lockdown. Clin Exp Optom. 2022;
Galvis V, Tello A, Otero J, Serrano AA, Gomez LM, Castellanos Y. Refractive errors in children and adolescents in Bucaramanga (Colombia). Arq Bras Oftalmol. 2017;80(6).
Morgan IG, Iribarren R, Fotouhi A, Grzybowski A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015;93(6).
Deng L, Gwiazda JE. Anisometropia in Children from Infancy to 15 Years. Invest Ophthalmol Vis Sci. 2012;53(7):3782–7.
Hu YY, Wu JF, Lu TL, Wu H, Sun W, Guo DD, et al. Prevalence and Associations of Anisometropia in Children. Invest Ophthalmol Vis Sci. 2016;57(3):979–88.
Signes-Soler I, Piñero DP, Murillo MI, Tablada S. Prevalence of visual impairment and refractive errors in an urban area of Mexico. Int J Ophthalmol. Oktober 20. 2019;12(19):1612–7.
Thom L, Jogessar S, McGowan SL, Lawless F. The prevalence and causes of decreased visual acuity – a study based on vision screening conducted at Enukweni and Mzuzu Foundation Primary Schools, Malawi. Clin Optom. 2017;9.
Lanca C, Saw S-M. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt. 2020;
Wen L, Cao Y, Cheng Q, Li X, Pan L, Li L, et al. Objectively measured near work, outdoor exposure and myopia in children. Br J Ophyhalmology. 2020;104:1542–1547.
Cao K, Wan Y, Yusufu M, Wang N. Significance of Outdoor Time for Myopia Prevention: A Systematic Review and Meta-Analysis Based on Randomized Controlled Trials. Ophthalmic Res. 2019;63(2):97–105.
Guan H, Yu NN, Wang H, Boswell M, Shi Y, Rozelle S. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS One. 2019;14(4):e021587.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2023 Willy Yahya, dr. Maria Larasati Susyono, Sp. M

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
