Management Ocular Syphilis in Human Immunodeficiency Virus (HIV) Patients
DOI:
https://doi.org/10.35749/journal.v48i1.100455Keywords:
Posterior Uveitis, Syphilis, HIV, neurosyphilisAbstract
Introduction: Ocular syphilis is a rare manifestation of syphilis. Ocular syphilis manifestations vary and can occur at all stages of the disease. Syphilis can affect all eye structures, the main complaint is blurred vision, accompanied by non-specific symptoms such as pain in the eye, and does not respond to steroids.
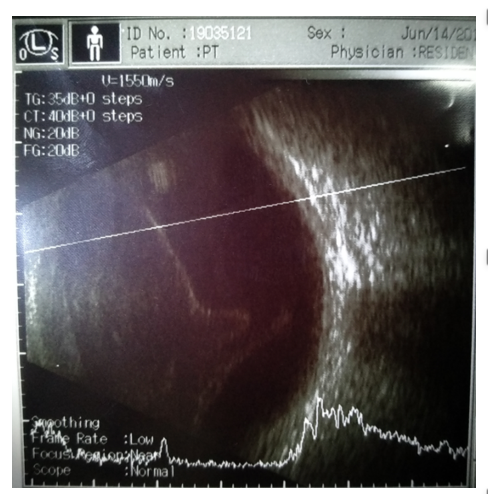
Case: The male patient, 54 years old, presents with complaints of both eyes slowly getting worse with a history of sexual multi-partners. Visual acuity in both eyes were light perception bad projection, ophthalmological examination showed cloudy lens, cloudy vitreous, cell (+) flare (+) right eye optic nerve, hyperemia, and left eye optic nerve, pale at temporal. VDRL results: reactive> 1: 512 and TPHA: reactive> 1: 5120. The patient was diagnosed with late latent syphilis and neurosyphilis observation from the Dermatology and Venereology Department and received benzathine penicillin injection therapy. From the Neurology Department the patient was diagnosed with neuro-syphilis and was consulted to VCT department with pre-HAART Stage IV HIV infection (WHO). After receiving penicillin therapy and topical steroids, the patient was experienced improvement in visual acuity.
Conclusion: In HIV patients without antiretroviral therapy, Treponema pallidum infection is more common and has manifestations such as ocular syphilis and neurosyphilis. Treatment of ocular syphilis using topical steroids to reduce inflammation and penicillin as the main antibiotic.
Downloads
References
Sitompul R. Diagnosis dan Penatalaksaan Uveitis dalam upaya Mencegah Kebutaan. Departermen Ilmu Kesehatan Mata FK Universitas Indonesia- RSCM. 2016. 4(1): (60)
Artini W. Uveitis dan Glaucoma: How to Diagnose Properly. Dipresentasi JEC@Saturday Seminar meeting. Jakarta, Indonesia. 2016
Benson CE, Soliman MK, Knezevic A, Xu DD, Nguyen QD, Do DV. Bilateral papillitis and unilateral focal chorioretinitis as the presenting features of syphilis. J Ophthalmic Inflamm Infect. 2015; 5:16
Sari KAD, Susila NKN, Budhiastra P. Karakteristik pasien uveitis di RSUP Sanglah Denpasar, periode Maret 2016 sampai Desember 2019. Jurnal Medika Udayana. 2019; 8(8): 1-7
Bollemeijer JG, Wieringa WG, Missotten TOAR, Meenken I, van Loon NHD, Rothova A, et al. Clinical Manifestations and Outcome of Syphilitic Uveitis. Rotterdam Eye Hospital, Rotterdam, The Netherlands. IOVS. 2016; 57(2): 404-411
Kanski,s Clinical Opthalmology, Eighth Edition, 2016 chapter 11(396)
Zhang T, Zhu Y, Xu G. Clinical Features and Treatments of Syphilitic Uveitis: A Systematic Review and Meta-Analysis. Journal of Ophthalmology. 2017; 1-16
American Academy of Opthalmology. Intraocular Inflammation and Uveitis. Basic and Clinical Science Course. Sec 9. San Fransisco. 2018-2019 (58)
Amode R, Makhloufi, S. Calin R, Caumes E. Oral doxycycline for syphilitic uveitis: a case report highlighting potential efficacy. J Antimicrob Chemother. 2018; 73: 1999–2000
Engelhard S, Patel V, Reddy A. Intermediate uveitis, posterior uveitis, and panuveitis in the Mid Atlantic USA. Clinical Ophthalmology. 2015; 9:1549–1555
Efrida E, Elvinawaty E. Imunopatogenesis Treponema pallidum dan Pemeriksaan Serologi. 2014; 3(3): 572-578
Elis Indira. Bagian / SMF Ilmu Kesehatan Kkulit dan Kelamin Fakultas Kedokteran UNUD / RS Sanglah Denpasar. 2016
Febrina D, Cahyawari D, Roslina N, Rowawi R, Achdiat PA. Laporan Kasus: Neurosifilis Asimtomatik Pada Pasien Sifilis Sekunder Dengan Koinfeksi Human Immunodeficiency Virus. Syifa’ MEDIKA. 2017; 8 (1): 1-10
World Health Organization. Guidelines for the Treatment of Treponema pallidum (syphilis). Geneva: WHO Document Production. 2016. (11)
American Academy of Opthalmology. Fundamentals. Basic and Clinical Science Course. Sec 9. San Fransisco. 2018-2019 (95)
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2022 Alexander Theodore Samosir, N. K. Niti Susila, I Gutsi Ayu Made Juliari, Ida Ayu Ary Paramita, I Made Agus Kusumadjaja

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
