Clinical Findings and Management of Angle Recession Glaucoma: A Case Report
DOI:
https://doi.org/10.35749/journal.v48i1.100255Keywords:
glaucoma, angle recession, combined phacoemulsification-trabeculectomyAbstract
Introduction: Angle recession is a common finding after blunt trauma and involves a tear between the longitudinal and circular fibers of ciliary body. The incidence of angle recession was 24.3%. It may occur months to years after ocular trauma.
Purpose: To report clinical findings and management of a patient with angle recession glaucoma.
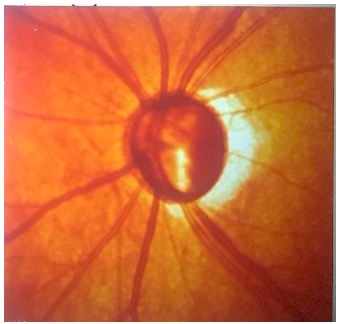
Case report: A 51 years old female came with chief complaint of blurry vision of left eye since five months earlier. There was a history of trauma in left eye 26 years ago. She had been treated with antiglaucoma medication by an ophthalmologist. Visual acuity of right eye was 1.0 and left eye was light perception. Applanation Tonometer Goldmann of left eye was 42 mmHg. Slit lamp examination revealed traumatic iritis and lens opacity. Gonioscopy revealed widening of ciliary body band in three quadrants. Funduscopy showed cup/disc ratio enlargement and RNFL thinning. This patient was diagnosed as angle recession glaucoma with traumatic iritis and traumatic cataract. Combined phacoemulsification-trabeculectomy with intraocular lens implantation was performed. One month after surgery, intraocular pressure decreased with improvement of visual acuity.
Conclusion: Classically clinical findings of angle recession glaucoma were unilateral glaucoma with history of trauma and widening of ciliary body band. Surgery is needed in uncontrolled intraocular pressure with medication. Combined phacoemulsification-trabeculectomy decreases intraocular pressure as well as improves visual acuity.
Downloads
References
Allingham RR. Shields Textbook of Glaucoma, 6th Edition. USA: Lippincott Williams & Wilkins; 2011.
American Academy of Ophthalmology. Glaucoma. Basic clinical science course: fundamentals and principles of opthalmology. Philadelphia USA: American Academy of Ophthalmology; 2016-2017.
Malik YK, Joel SS, David LE. Chandler and Grants Glaucoma, 5th Edition. USA: SLACK Incorporated; 2013.
Careti L, Buratto L. Glaucoma surgery treatment and technique. Switzerland: Springer International Publishing AG; 2018.
Maity P, dkk. Incidence of angle recession after blunt trauma- A longitudinal study. Indian Journal of Clinical and Experimental Ophthalmology; January - March 2018; 4(1): 136 – 140.
Ajite KO, dkk. Survey of Traumatic Glaucoma in a Tertiary Hospital. Journal of Trauma and Treatment; March 2017, 6:1.
Sihota R, dkk. Early Predictors of Traumatic Glaucoma After Closed Globe Injury; (Reprinted) Arch Ophthalmol/Vol 126 (No. 7), July 2008. Downloaded From: http://archopht.jamanetwork.com/ by a University of Sussex Library User on 08/10/2015.
Asia Pacific Glaucoma Society. Asia Pacific Glaucoma Guidelines. Netherland: Kugler Publications; 2016.
Gunvant P. Glaucoma – Current Clinical and Research Aspects. Croatia: Intechopen; 2011.
Clement CI, Goldberg I. The management of complicated glaucoma; January 2011; 59 Suppl: S141-7.
Choy BNK. Comparison of surgical outcome of trabeculectomy and phacotrabeculectomy in Chinese glaucoma patients. International Journal of Ophthalmology; 2017;10(12):1928-1930.
Singh K, Dangda S. Ocular trauma: Post traumatic glaucoma. DOS Times; February 2015; 20(8).
Ahmed IIK, dkk. Mitomycin, MIGS, and Microstents: The Role of Antimetabolites in Glaucoma Surgery. MedEdicus; December 2017.
Downloads
Published
License
Copyright (c) 2022 Madona Debora, Maulida Rifada, Andika Prahasta, Elsa Gustianty

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
