AUROLAB AQUEOUS DRAINAGE IMPLANT IN YOUNG ADULT WITH NEOVASCULAR GLAUCOMA AND TUBERCULOSIS HISTORY: A CASE REPORT
DOI:
https://doi.org/10.35749/journal.v49i1.100170Keywords:
AADI, Neovascular glaucoma, TuberculosaAbstract
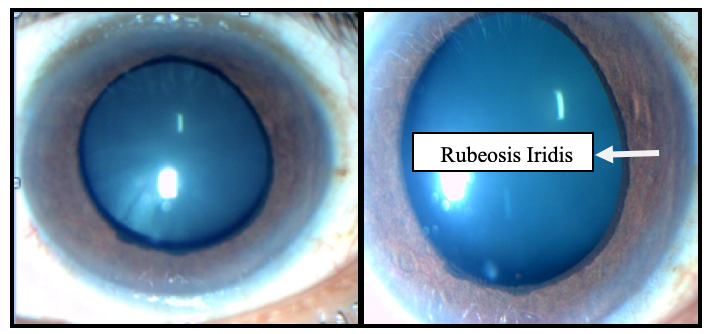
Introduction: Neovascular glaucoma (NVG) is historically known as rubeotic glaucoma, from “rubeosis iridis” that refers to the iris neovascularization. One of several causes that lead to rubeosis iridis is changes in Pigment Epithelium-Derived Growth Factor (PEDF) that may be caused by Mycobacterium tuberculosis. The influence of NVG may cause intraocular pressure (IOP) to rise rapidly. It can be decreased by Aurolab Aqueous Drainage Implant (AADI).
Case Report: A 34-year-old male complained of left eye pain and sudden decreased vision for the past 2 months. He had been diagnosed with tuberculosis since 8 months ago. The patient’s blood pressure, blood sugar, cholesterol, and triglycerides were within normal limit. Diabetes Mellitus (-). Human Immunodeficiency Virus (-). Visual acuity of left eye was hand movement. The pupil was dilated and non-reactive, anterior chamber depth is shallow, and rubeosis iridis (+). IOP is 60 mmHg. Medical management was failed to decrease the IOP. Funduscopy image showed cup-disc ratio was 0,7. Ganglion cell complex parameters showed 80,91. On the next day after AADI implantation surgery, the patient’s left eye IOP was reduced to 10 mmHg. On the 14th day post operative visual acuity was 2 meter counting finger. The anterior segment of the conjunctiva bulbi was hyperemic and conjunctival injection was reduced. The camera oculi anterior showed remainder of the implant. In the iris, rubeosis iridis disappeared, pupil was dilated, IOP was increased to 12 mmHg
Discussion: Neovascular glaucoma was caused by the growth of the fibrovascular membrane on the surface of the iris and the anterior chamber angle. The three most common causes of neovascular glaucoma were diabetes mellitus, central retinal vein occlusion, and carotid artery occlusion.
Conclusion:AADI is a safe and effective option for patients with neovascular glaucoma following tuberculosis.
Downloads
References
Rhee D.J, Nicholl. Secondary Angle Closure Glaucoma. Glaucoma. 2003;17:326-328.
Khan Y.A. Glaucoma Neovascular. 2006.
Vaughan, Asbury S. Neovascular Glaucoma. General Ophthalmology 6th Ed. 2006;212-27.
William L & Wilkins. 2005. Glaucomas Asscociated With Disorder of the Retina, Vitreous and Choroid in Shields. Glaucoma 5th Ed; 2005. 19: pp. 328-37.
American Academy of Ophthalmology. Basic and Clinical Science Course section 10: Glaucoma. San Fransisco : American Academy of Ophthalmology. 2018.
Mosby. Mosby's Medical Dictionary, Amsterdam: Elsevier 8th Ed; 2008.
Ilyas S, Tanzil M. Glaukoma. Ilmu Penyakit mata 3rd Ed. Jakarta: Balai Penerbit FKUI; 2006. p.212-18
Wijaya N. Glaukoma Sekunder. Ilmu Penyakit Mata. Jakarta : Balai Penerbit FKUI; 2008; 219-44.
Bertamian M. Glaucoma Neovascular in Clinical Guide to Glaucoma Management. Amsterdam: Elsevier; 2004;263-9.
Madhavan HN, Therese KL, Kavitha D. Further investigations on the association of Mycobacterium tuberculosis with Eales’ disease. Indian J Ophthalmol. 2002; 50:35–39.
Bhutto IA, McLeod DS, Hasegawa T, et al. Pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in aged human choroid and eyes with age-related macular degeneration. Exp Eye Res. 2006;82(1):99-110.
Saxena S, Pant AB, Khanna VK, et al. Interleukin-1 and tumor necrosis factor-alpha: novel targets for immunotherapy in Eales disease. Ocul Immunol Inflamm. 2009;17(3):201-206.
Sen A, Chowdhury IH, Mukhopadhyay D, et al. Increased Toll-like receptor-2 expression on nonclassic CD16+ monocytes from patients with inflammatory stage of Eales' disease. Invest Ophthalmol Vis Sci. 2011;52(9):6940-6948.
Cosgrove GP, Brown KK, Schiemann WP, et al. Pigment epithelium-derived factor in idiopathic pulmonary fibrosis: a role in aberrant angiogenesis. Am J Respir Crit Care Med. 2004;170(3):242-251.
Liu JT, Chen YL, Chen WC, et al. Role of pigment epithelium-derived factor in stem/progenitor cell-associated neovascularization. J Biomed Biotechnol. 2012:871272.
Li X, Wang T, Yang T, et al. Elevated plasma levels of pigment epithelium-derived factor correlated with inflammation and lung function in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10:587-594.
Ogata N, Tombran-Tink J, Nishikawa M, et al. Pigment epithelium-derived factor in the vitreous is low in diabetic retinopathy and high in rhegmatogenous retinal detachment. Am J Ophthalmol. 2001;132(3):378-382.
Boehm BO, Lang G, Volpert O, et al. Low content of the natural ocular anti-angiogenic agent pigment epithelium-derived factor (PEDF) in aqueous humor predicts progression of diabetic retinopathy. Diabetologia. 2003;46(3):394-400..
Angayarkanni N, Selvi R, Pukhraj R, Biswas J, Bhavesh SJ, Tombran-Tink J. Ratio of the vitreous vascular endothelial growth factor and pigment epithelial-derived factor in Eales disease [published correction appears in J Ocul Biol Dis Infor. 2009 Jun;2(2):94]. J Ocul Biol Dis Infor. 2009;2(1):20-28.
Tiwari A, Trivedi AC, Srivastava P, Pant AB, Saxena S. Comparative modeling of retinol-binding protein-3 and retinal S-antigen in Eales' disease and prediction of their binding sites using computational methods. J Ocul Biol Dis Infor. 2010;3(3):88-91
Li X, Wang T, Yang T, Shen Y, An J, Liu L, Dong J, Guo L, Li D, Zhang X, Chen L, Xu D, Wen F. Elevated plasma levels of pigment epithelium-derived factor correlated with inflammation and lung function in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10(1):587-594.
Mishra A, Luthra S, Baranwal VK, Parihar JK. An interesting case of rubeosis iridis with neovascular glaucoma in a young patient. Med J Armed Forces India. 2013;69(2):187-189.
Ravi, K., Srivastava, P., Movdawalla, M., Sen, S., and Kedia, P. 2017. Implants in glaucoma: a minor review. Sci J Med & Vis Res Foun. Vol. XXXV:3-9.
Teruhiko H, Takayasu O, Noriko A, Toshiro Y, and Nobuo I. 2012. Retinal Photocuagulation Density in the Treatment of Neovascular Glaucoma due to Diabetic Retinopathy
Archana S, Premanand C, Raman GV. Aurolab aqueous drainage implant: My surgical technique. Kerala J Ophthalmol 2017;29:41-5.
Stein JD. Standard technique for implanting glaucoma drainage devices. Essentials of Glaucoma Surgery. 1st ed. 2002. New Jersey: Slack Inc.; pp.81-94.
Downloads
Published
License
Copyright (c) 2023 Barii Hafidh Pramono, Masitha Dewi Sari, Aslim D. Sihotang

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
