Cataract Surgery After Keratoplasty: How Should We Prepare?
Poster Presentation - Case Series - Resident
DOI:
https://doi.org/10.35749/5xx1gd17Keywords:
Keratoplasty, cataract surgery, IOL calculation, phacoemulsificationAbstract
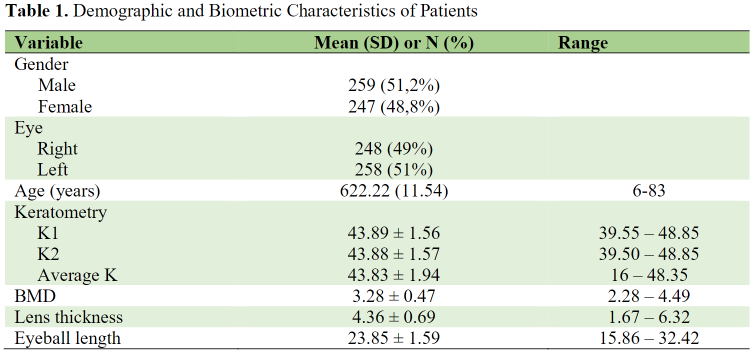
Introduction : Cataract surgery following corneal transplantation demands special attention to corneal graft stability and optimization to allow for excellent IOL selection, as well as corneal graft preservation since lens removal damages the corneal endothelium. This study aimed to determine how we should prepare for cataract surgery after keratoplasty.
Case Illustration : Case 1: A 34-year-old male has phacoemulsification in his right eye (last eye). He had a history of eye surgery, including, keratoplasty for RE in 2019, and vitrectomy for RE because of endophthalmitis. The pre-operative visual acuity is 0.5/60 with PAS and an irregular pupil. Post-operative VA 3/60 with BCVA 6/40. Last follow-up, the grafted cornea was still clear with normal IOP. Case 2: A 50- year-old female underwent phacoemulsification for both eyes (BE). She had histories of keratoplasty in 1986, 1989, and 1997 for BE. She also had extreme myopia for BE (RE S -17.00, LE S-14.00). Pre- operative VA was 1/60 of BE, and BCVA was 6/20 a month after surgery. During the last check-up, both transplant corneas were clear with normal IOP. Last visit, her both grafts remained clear.
Discussion :
Conclusion : IOL calculations are challenging due to inaccuracy in corneal measurements, astigmatism, or corneal pathology. The best time to perform surgery is at least 2 years after keratoplasty. We suggest using total keratometry in the K-6 formula or Haigis for the IOL formula. Good dispersive viscoelastic, operating away from the corneal endothelium, and employing low phaco-energy/fluids will help to deliver a clear cornea after surgery. Last, steroid treatment will enhance graft survival rate.
Downloads
References
(-)
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.