AN ATYPICAL CASE OF BILATERAL CORNEAL OPACITY: WHAT ARE THE POSSIBLE DIAGNOSIS?
DOI:
https://doi.org/10.35749/c1s1j485Keywords:
corneal keloid, subclinical infection, rare diseaseAbstract
Introduction: Corneal opacity can be divided into inflammatory and noninflammatory entities. The clinical presentation and characteristics of a corneal opacity can often help reach a diagnosis. However, atypical cases are more challenging to diagnose. This report aims to explore an atypical case of corneal opacity and the diagnostic approach through its clinical presentation.
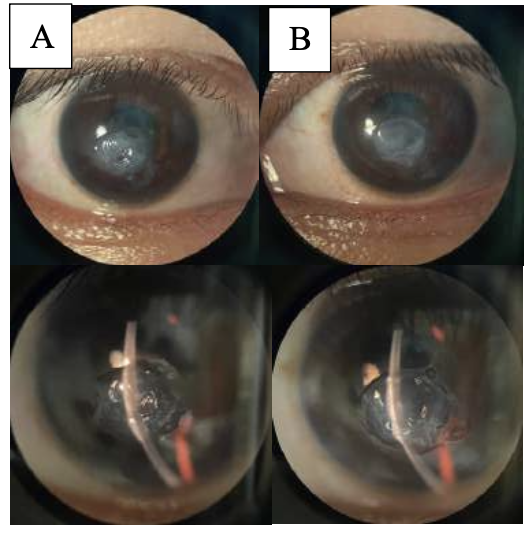
Case Report: A thirty-seven-year-old female patient had a chief complaint of gradual blurry vision in both eyes and slowly growing whitish lesions one year prior. The patient recalled a history of bilateral eye redness two years ago. The anterior segment examination and AS-OCT revealed bilateral, smooth, oedematous pearly-white elevated opacity with well-demarcated margins at the center of the cornea, with epithelial depth. The diagnosis of corneal keloid was favored, with GDLD and SND as the differential diagnosis. In local anesthesia, the patient underwent superficial keratectomy and amniotic membrane transplantation of the right eye. On one month follow-up, the patient felt an improvement in her subjective complaints with a normal appearance of the cornea.
Discussion: The atypical characteristics found in our case didn’t fit a single mold, as it shared features of post- injury hypertrophic scar, degenerative, and dystrophy. We diagnosed the patient with corneal keloid caused by suspicion of subclinical infection. Although GDLD and SND were still possible, the working diagnosis was enough to warrant a therapeutic surgical removal.
Conclusion: Atypical presentations make diagnosis more challenging. However, despite improvements in diagnostic modalities, signs, and symptoms remain very helpful in reaching a working diagnosis.
Downloads
References
Gupta J, Gantyala SP, Kashyap S, et al. Diagnosis, management, and histopathological characteristics of corneal keloid: a case series and literature review. Asia Pac J Ophthalmol. 2016.
Vu CV, Hwang FS. Corneal keloids. eyewiki.aao.org. Updated 2022 Apr 10. Accessed June 29, 2022.
AAO 2021-2022. Basic and clinical science course, section 8: external disease and cornea. 2021.
Vanathi M, Panda A, Kai S, et al. Corneal keloid. The Ocular Surface. 2008;6(4):186-97.
Bakhtiari P, Agarwal DR, Fernandez AA, et al. Corneal keloid: report of natural history and outcome of surgical management in two cases. 2013 Dec;32(12):1621-4.
Miyamoto R, Sakimoto T, Homma T, et al. A rare case of corneal keloid occurred 30 years after pterygium surgery and 3 years after cataract surgery. Am J Ophthalmol Case Rep. 2020.
Siebelmann S, Scholz P, Sonnenschein S, Bachmann B, Matthaei M, Cursiefen C, et al. Anterior segment optical coherence tomography for the diagnosis of corneal dystrophies according to the IC3D classification. Surv Ophthalmol. 2017.
Sridhar MS, Martin R. Anterior segment optical coherence tomography for evaluation of cornea and ocular surface. Indian J Ophthalmol. 2018;66:367-72.
Brown AC, Nataneli N. Salzmanns nodular corneal degeneration. Treasure Island: StatPearls Publishing;2023 Jan.
Patel AS, Akkara JD, DelMonte DW, Morkin M, Murchison A, Alexander JL. Ultrasound biomicroscopy.eyewiki.aao.org. Updated 2023 Mar 21. Accessed August 2023.
Hsieh M-C, Huang J-Y, Liu Y-L, et al. Bilateral corneal keloids after eyelid compression. Taiwan J Opthalmol. 2020;10:58-61.
Deshmukh R, Reddy JC, Rapuano CJ, et al. Phototherapeutic keratectomy: indications, methods and decision making. Indian J Ophthalmol. 2020;68:2856-66.
Lee HK, Choi HJ, Kim MK, et al. Corneal keloid: four case reports of clinicopathological features and surgical outcome. BMC Ophthalmology. 2016;16:198.
Palko JR, Arfeen S, Farooq AV, et al. Corneal keloid presenting forty years after penetrating injury: case report and literature review. Surv Ophthalmol. 2019.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Jessica Zarwan, Astrid Mariam Khairani Siregar, Marsha Rayfa Pintary, Syska Widyawati, Faraby Martha, Rio Rhendy

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
