NEUROOPHTHALMOLOGIC MANIFESTATIONS AMONG 195 PATIENTS WITH INTRACRANIAL TUMOR AT NATIONAL REFERRAL HOSPITAL
DOI:
https://doi.org/10.35749/r4yg5d37Keywords:
Intracranial tumor, Brain tumor, Blindness, Optic atrophy, HemianopiaAbstract
Introduction & Objective: Intracranial tumor might show neuroophthalmological manifestations. Early detection and prompt treatment could alter the visual outcome. Ophthalmologists need to be aware of neuroophthalmological features commonly found among patients with intracranial tumor. This study revealed those signs and symptoms.
Methods: Study was done in tertiary referral hospital. Subjects were patients with intracranial tumor attending neuroophthalmology clinic between the specified period. It was a descriptive study using retrospective data of the patient’s initial visit to the clinic. Data was retrieved from the medical record archive and electronic health record.
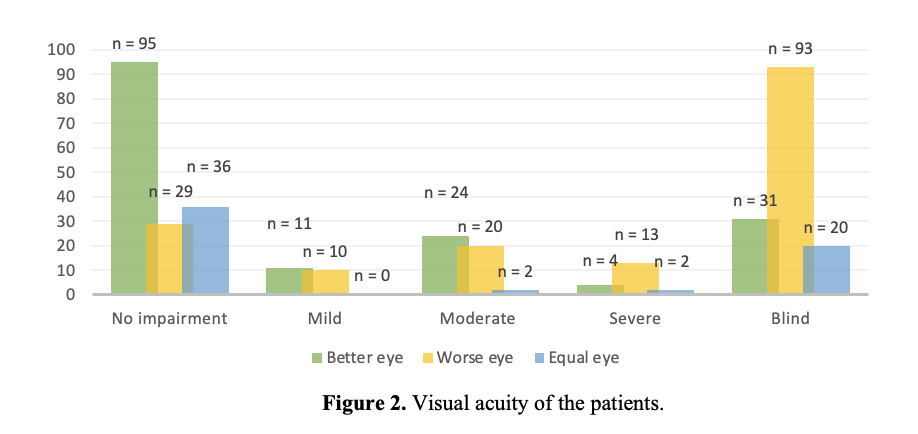
Results : There were 195 patients, 67.7% of them were women, with average age 43.4 years old. Half the patients arrived within 6 months after eye related symptoms occurred and the referring physicians was equal between ophthalmologists and other specialties. The most frequent symptom and sign were blurred vision and optic nerve head abnormality (atrophy, edema). Hemianopia outnumbered other patterns of visual field disturbance, yet bilateral pattern was difficult to be evaluated as most patients had either one or both eyes blind.
Conclusion : Intracranial tumor was one of the diseases that could show ophthalmic signs and symptoms. Neuroophthalmological manifestations in those cases was related to the extraocular process and the relevant pathway affected by the tumor.
Downloads
References
American Association of Neurological Surgeon. Brain Tumors. [Internet] Accessed October 26, 2021. Available at: https://www.aans.org/en/Patients Neurosurgical-Conditions-and-Treatments/Brain-Tumors.
Goshtasbi K, Abiri A, Sahyouni R, Mahboubi H, Raefsky S, Kuan EC, et al. Visual and endocrine recovery following conservative and surgical treatment of pituitary apoplexy: A meta-analysis. World Neurosurg. 2019;132:33-40.
Kitthaweesin K, Ployprasith C. Ocular manifestations of suprasellar tumors. J Med Assoc Thai. 2008;91(5):711-5.
Pelsma ICM, Verstegen MJT, de Vries F, Notting IC, Broekman MLD, van Furth WR, et al. Quality of care evaluation in non-functioning pituitary adenoma with chiasm compression: visual outcomes and timing of intervention clinical recommendations based on a systematic literature review and cohort study. Pituitary. 2020;23(4):417-29.
Muskens IS, Zamanipoor Najafabadi AH, Briceno V, Lamba N, Senders JT, van Furth WR, et al. Visual outcomes after endoscopic endonasal pituitary adenoma resection: a systematic review and meta-analysis. Pituitary. 2017;20(5):539-52.
Jahangiri A, Lamborn KR, Blevins L, Kunwar S, Aghi MK. Factors associated with delay to pituitary adenoma diagnosis in patients with visual loss. J Neurosurg. 2012;116(2):283-9.
World Health Organization. Blindness and Visual Impairment. [Internet] Accessed November 14, 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment
Desmukh S, Das D, Bhattacharjee H, Kuri GC, Magdalene D, Gupta K, et al. Profile of brain tumors having ocular menifestations in a tertiary eye care institute: A retrospective study. TNOA J Ophthalmic Sci Res 2018;56:71-5.
Sefi-Yurdakul N. Visual findings as primary manifestations in patients with intracranial tumors. Int J Ophthalmol. 2015;8(4):800-3.
Tagoe NN, Essuman VA, Fordjuor G, Akpalu J, Bankah P, Ndanu T. Neuro-ophthalmic and clinical characteristics of brain tumours in a tertiary hospital in Ghana. Ghana Med J. 2015;49(3):181-6.
Zheng J, Chen W, Huang D, Wang Y, Zheng D, Zhou L, et al. Ocular symptoms as the initial clinical manifestations in patients with extraocular tumors. Ann Transl Med. 2021;9(6):497.
Bondy ML, Scheurer ME, Malmer B, Barnholtz-Sloan JS, Davis FG, Il'yasova D, et al. Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer. 2008;113(7 Suppl):1953-68.
Walsh KM, Kelsh EB, Wrensch MR. Epidemiology. In: Bernstein M, Berger MS. Neuro-Oncology: The Essentials, 3rd ed. Thieme: New York; 2015.
Barnholtz-Sloan JS, Kruchko C. Meningiomas: causes and risk factors. Neurosurg Focus. 2007;23(4):E2.
Dhivya R. Neuro-ophthalmic manifestations of intracranial tumours: A clinical profile. [Dissertation] The Tamilnadu Dr. MGR Medical University; 2014.
Onakpoya OH, Komolafe EO, Akintomide F, Ajite K, Komolafe MA, Adeolu AA, et al. Ophthalmic manifestations in patients with intracranial tumours. African Journal of Neurological Sciences. 2009;28(1):55-62.
Khan A, Khan S, Khan M. Factors effecting life expectancy in developed and developing countries of the world (An approach to available literature). International Journal of Physical Education and Sports. 2016;1(1):4-6.
Astorga-Carballo A, Serna-Ojeda JC, Camargo-Suarez MF. Chiasmal syndrome: Clinical characteristics in patients attending an ophthalmological center. Saudi J Ophthalmol. 2017;31(4):229-33.
Hu CX, Zangalli C, Hsieh M, Gupta L, Williams AL, Richman J, dkk. What do patients with glaucoma see? Visual symptoms reported by patients with glaucoma. Am J Med Sci. 2014;348(5):403-9.
Ravn Munkvold BK, Sagberg LM, Jakola AS, Solheim O. Preoperative and postoperative headache in patients with intracranial tumors. World Neurosurg. 2018;115:e322-e30.
Hadidchi S, Surento W, Lerner A, Liu CJ, Gibbs WN, Kim PE, et al. Headache and brain tumor. Neuroimaging Clin N Am. 2019;29(2):291-300.
Verma R, Gupta M, Chaudhari TS. Neurogenic vision loss: Causes and outcome. An experience from a tertiary center in Northern India. J Neurosci Rural Pract. 2014;5(4):340-8.
Vié AL, Raverot G. Modern neuro-ophthalmological evaluation of patients with pituitary disorders. Best Pract Res Clin Endocrinol Metab. 2019;33(2):101279.
Vejdani A. Relative Afferent Pupillary Defect. [Internet] Accessed December 20, 2021. Available at: https://eyewiki.aao.org/Relative_Afferent_Pupillary_Defect
Ahmad SS, Kanukollu VM. Optic Atrophy. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559130/
Foroozan R BM, Falardeau J, Gordon LK, Lee MS, Subramanian PS, et al. The Patient with Decreased Vision: Evaluation. 2016. In: Neuro-Ophthalmology [Book]. 2016-2017. Basic Clinical and Science Course.
Cosetti MK, Tawfik K, Fouladvand M, Roland JT, Lalwani AK. Diplopia due to skew deviation following neurotologic procedures. Otol Neurotol. 2012;33(5):840-2.
Larjavaara S, Mäntylä R, Salminen T, Haapasalo H, Raitanen J, Jääskeläinen J, et al. Incidence of gliomas by anatomic location. Neuro Oncol. 2007;9(3):319-25.
American Association of Neurological Surgeon. Meningiomas. [Internet] Accessed December 16, 2021. Available at: https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Meningiomas
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Dita Permatasari, Syntia Nusanti

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
