The VARIATION OF THE AXIAL LOCATION OF BRUCH’S MEMBRANE OPENING, GANGLION CELL INNER PLEXIFORM LAYER AND FLUX INDEX IN NORMAL TENSION GLAUCOMA AND PRIMARY OPEN ANGLE GLAUCOMA PATIENTS
DOI:
https://doi.org/10.35749/journal.v49i2.100660Keywords:
Bruch’s membrane opening (BMO), Normal Tension Glaucoma, Primary Open Angle GlaucomaAbstract
Introduction. Bruch’s membrane opening (BMO) at the most anterior point of the neural canal for quantification of cup depth /based on retinal surface position, area and volume, laminar position, and prelaminar connective tissue volume. If these deep structural parameters are to be used effectively in glaucoma detection and identification of progression.
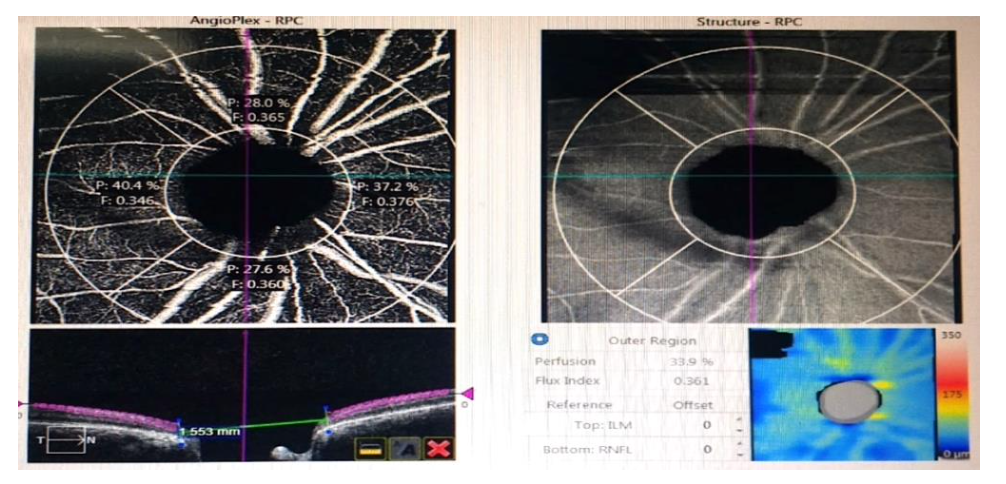
Purpose. This study explores variation in the axial location of Bruch’s membrane opening (BMO) to determine if this reference plane varies with NTG and POAG patients.
Methods This was a cross-sectional prospective descriptive study with purposive sampling. This study enrolled 72 eyes in Sardjito General Hospital underwent cirrus – OCT 5000 Ver 11.0.0.29946 between 1st March 2022 and 10th May 2022.
Results. We evaluated 72 (25 NTG and 47 POAG) eyes on 37 outpatients service of Sardjito General Hospital. Median BMO, GCIPL, Flux index and CD ratio of NTG patients was 1.707 µm (1.387-2.182), 83,0µm (76-88), 0,40 (0.27-0,48), 0,64 (0,22-0,75). Median BMO, GCIPL, Flux index and CD ratio of POAG patients was 1.612 (1.028-2.031) µm, 79,00 (56-98) µm, 0,40 (0,26-0,47) and 0,64 (0,28-0,92) for CDR. Bruch’s membrane opening position was more posterior relative to the sclera in older subjects with negative correlation (P value = 0,07). Variable BMO and GCIPL tested between NTG and POAG group showed significant difference with BMO P value =0,04 and GCIPL P value=0,01 except Perfusion, flux index and RNFL.
Conclusion. Bruch’s membrane opening is more posteriorly located in older individuals. There was significant difference p value of BMO between the mean of NTG and POAG.
Downloads
References
Weinreb R. N., Khaw P. T., “Primary open-angle glaucoma,” The Lancet 363, 1711–1720 (2004). 10.1016/S0140-6736(04)16257-0
Yousefi S., Goldbaum M. H., Balasubramanian M., Jung T., Weinreb R. N., Medeiros F. A., Zangwill L. M., Liebmann J. M., Girkin C. A., Bowd C., “Glaucoma progression detection using structural retinal nerve fiber layer measurements and functional visual field points,” IEEE Transactions on Biomed. Eng. 61, 1143–1154 (2014). 10.1109/TBME.2013.2295605
Pusdatin Kemenkes. 2019. Situasi Glaukoma di Indonesia. https://pusdatin.kemkes.go.id/article/view/19080500002/situasi-glaukoma-di-indonesia.html
Mwanza J.-C., Chang R. T., Budenz D. L., Durbin M. K., Gendy M. G., Shi W., Feuer W. J., “Reproducibility of peripapillary retinal nerve fiber layer thickness and optic nerve head parameters measured with cirrus hd-oct in glaucomatous eyes,” Investig. Ophthalmol. & Vis. Sci. 51, 5724 (2010). 10.1167/iovs.10-5222
Manassakorn A., Nouri-Mahdavi K., Caprioli J., “Comparison of retinal nerve fiber layer thickness and optic disk algorithms with optical coherence tomography to detect glaucoma,” Am. J. Ophthalmol. 141, 105–115.el (2006). 10.1016/j.ajo.2005.08.023
Belghith A., Bowd C., Medeiros F. A., Hammel N., Yang Z., Weinreb R. N., Zangwill L. M., “Does the location of bruch’s membrane opening change over time? longitudinal analysis using san diego automated layer segmentation algorithm (salsa),” Investig. Ophthalmol. & Vis. Sci. 57, 675 (2016). 10.1167/iovs.15
Strouthidis, N. G., Yang, H., Downs, J. C. & Burgoyne, C. F. Comparison of clinical and three-dimensional histomorphometric optic disc margin anatomy. Invest Ophthalmol Vis Sci. 50, 2165–2174 (2009).
Jonas, J. B. & Xu, L. Histological changes of high axial myopia. Eye (Lond). 28, 113–117 (2014)
Jonas, J. B., Holbach, L. & Panda-Jonas, S. Peripapillary ring: histology and correlations. Acta Ophthalmol. 92, e273–e279 (2014).
Chauhan, B. C. & Burgoyne, C. F. From clinical examination of the optic disc to clinical assessment of the optic nerve head: a paradigm change. Am J Ophthalmol. 156, 218–227 (2013).
Kim, M., Choung, H. K., Lee, K. M., Oh, S. & Kim, S. H. Longitudinal changes of optic nerve head and peripapillary structure during childhood myopia progression on OCT: Boramae Myopia Cohort Study report 1. Ophthalmology. 125, 1215–1223 (2018).
Chauhan BC, Burgoyne CF. From clinical examination of the optic disc to clinical assessment of the optic nerve head: a paradigm change. Am J Ophtalmol. 2013; 156: 218-227.
Reus NJ, Lemij HG. Relationships between standard automated perimetry HRT confocal scanning laser ophthalmoscopy, and GDx VCC scanning laser polarimetry. Invest Ophthalmol Vis Sci. 2005; 46: 4182–4188.
Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol. 2009; 127: 1250–1256.
Reus NJ, Lemij HG. The relationship between standard automated perimetry and GDx VCC measurements. Invest Ophthalmol Vis Sci. 2004; 45: 840–84
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2023 Jehan Fauzi Jehan, Retno Ekantini, Tatang Talka Gani, Krisna Dwi Purnomo Jati

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
