Effect of Phacotrabeculectomy on Ocular Biometric, Gonioscopic and Intraocular Pressure In Patients With Primary Angle Closure Glaucoma
DOI:
https://doi.org/10.35749/journal.v48i1.100496Keywords:
PACG, phacotrabeculectomy, ocular biometrics, gonioscopic, intraocular pressureAbstract
Objectives: The objective of this study is to have an expanded evaluation on the effect of phacotrabeculectomy on ocular biometric (ACD/anterior chamber depth, lens thickness), gonioscopic and intraocular pressure (IOP) in primary angle closure glaucoma (PACG).
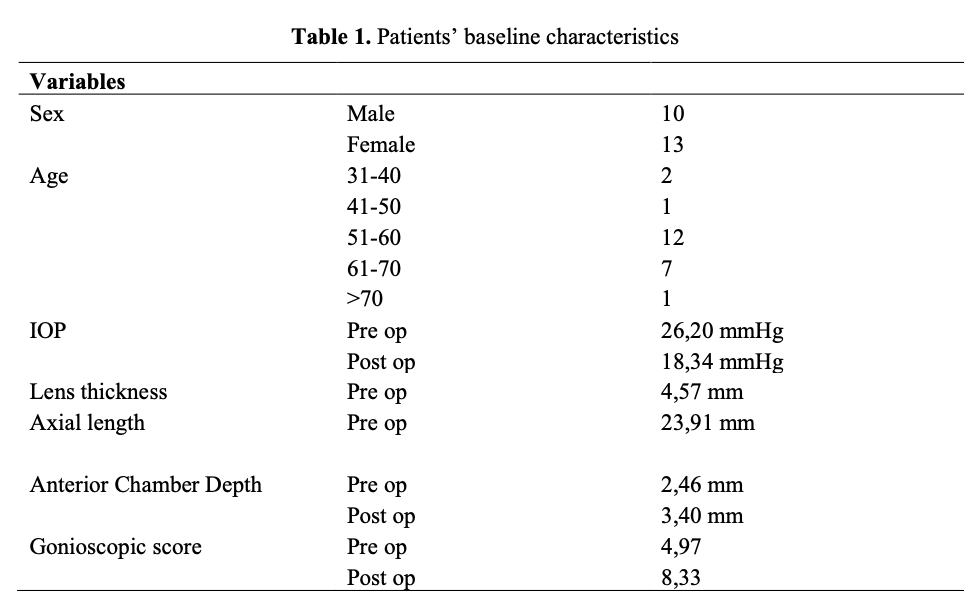
Methods: A cohort study of PACG patient who underwent phacotrabeculectomy from September 2018- March 2019 at Dr.Kariadi hospital. Preoperative secondary data of baseline IOP, ACD, lens thickness, and gonioscopy were obtained from medical record. Postoperative primary data of IOP, ACD, and gonioscopy were obtained 2 weeks after surgery.
Results: Thirty eyes from 23 patients had preoperative and postoperative mean IOP (26,20±2,24 and 18,35±2,49), mean ACD (2,46±0,37 and 3,40±0,40), mean gonioscopic score (4,97±0,96 and 8,33±1,63), mean preoperative lens thickness (4,58±0,39). There were significant differences between IOP, ACD and gonioscopic score (<0,001) before and after phacotrabeculectomy. The greater lens thickness was associated with IOP reduction ( <0,001 r=0,756), increased ACD ( 0,005 r=0,498), and increased gonioscopic score ( <0,001, r=0,802). The positive correlation can be seen between gonioscopic score and ACD ( <0,001 r=0,666) and the negative correlation between IOP and ACD ( <0,001 r=0.683), IOP and gonioscopic score ( <0,001 r=0,876).
Conclusion: Phacotrabeculectomy may be effective in reducing IOP, increasing ACD, and gonioscopic scores significantly in PACG patients. Lens thickness may be positively
Downloads
References
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002; 86: 240-241. Available at: http://www.ncbi.nlm. nih.gov/pmc/articles/PMC1771026/pdf/bjo08600238.pdf. Accessed June 15,2019
Fea, Antonio, Bertaina, Lorella, Angle Closure Glaucoma: Pathogenesis and Evaluation. A Review, Journal of Clinical & Experimental Ophthalmology, January 2012: 1-2 DOI: 10.4172/2155-9570.S4-005
Hejtmancik, J Fielding et al. “Lens Biology and Biochemistry.” Progress in molecular biology and translational science vol. 134 (2015): 169-201. doi:10.1016/bs.pmbts.2015.04.007
Li, Hai-Jun et al. “Comparison Of Phacotrabeculectomy And Sequential Surgery In The Treatment Of Chronic Angle- Closure Glaucoma Coexisted With Cataract.” International journal of ophthalmology vol. 9,5 687-92. 18 May. 2016, doi:10.18240/ijo.2016.05.08
Poon, L., Lai, I., Lee, J., Tsai, J., Lin, P. and Teng, M. (2015). Comparison of surgical outcomes after phacotrabeculectomy in primary angle-closure glaucoma versus primary open-angle glaucoma. Taiwan Journal of Ophthalmology, 5(1), pp.28-31.
Hai, jun Li, Xiao-MinZhu. (2016) Comparison of phacotrabeculectomy and sequential surgery in the treatment of chronic angle-closure glaucoma coexisted with cataract. International Journal Ophthalmology. www. ijo. Cn
Bilak, S., Simsek, A., Capkin, M., Guler, M. and Bilgin, B. (2015). Biometric and Intraocular Pressure Change after Cataract Surgery. Optometry and Vision Science, 92(4), pp.464-470.
Sihota R, Gupta V, Agarwal HC, Pandey RM, Deepak KK. Comparison of symptomatic and asymptomatic, chronic, PACG, open-angle glaucoma, andcontrols. J Glaucoma 2000; 9:211–213
Jahn CE. Reduced intraocular pressure after phacoemulsification and posterior chamber intraocular lens implantation.J Cataract Refract Surg 1997; 23:1262–1264
Sacca` S, Marletta A, Pascotto A, Barabino S, Rolando M, Giannetti R, Calabria G. Daily tonometric curves after cataract surgery. Br J Ophthalmol 2001; 85:27–29. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1723696/pdf/v085 p00024. pdf. Accessed April 24, 2019
Schwenn O, Dick HB, Krummenauer F, Krist R, Pfeiffer R. Intraocular pressure after small incision cataract surgery: temporal sclerocorneal versus clear corneal incision. J Cataract Refract Surgery 2001; 27:421–425
Lai JSM, Tham CCY, Chan JCH, Lam DSC. Phacotrabeculectomy in treatment of primary angle-closure glaucoma and primary open-angle glaucoma. Jpn J Ophthalmol. 2004;48:408e411.
Rao HL, Maheshwari R, Senthil S, Prasad KK, Garudadri CS. Phacotrabeulectomy without mitomycin c in primary angle-closure and open- angle glaucoma.J Glaucoma. 2011;20:57e62.
Tong JT, Miller KM. Intraocular pressure change after sutureless phacoemulsification and foldable posterior chamber lens implantation.J Cataract Refract Surg 1998; 24:259–261
Hayashi K, Hayashi H, Nakao F, Hayashi F. Effect of cataract surgery on intraocular pressure control in glaucoma patients. J Cataract Refract Surg 2001; 27:1779–1786
Hayashi K, Hayashi H, Nakao F, Hayashi F. Changes in anterior chamber angle width and depth after intraocular lens implantation in eyes with glaucoma. Ophthalmology 2000; 107: 700–702
Gunning FP, Greve EL. Lens extraction for uncontrolled angleclosure glaucoma: long-term follow-up. J Cataract Refract Surg 1998; 24:1347–1356
Poley BJ, Lindstrom RL, Samuelson TW, Schulze R Jr. Intraocular pressure reduction after phacoemulsification with intraocular lens implantation in glaucomatous and nonglaucomatous eyes: evaluation of a causal relationship between the natural lens and open-angle glaucoma. J Cataract Refract Surg 2009; 35:1946–1955
Ekic¸ O, Batman C. Effect of capsulorhexis size on postoperative intraocular pressure. J Cataract Refract Surg 1999; 25: 416–419
Meyer MA, Savitt ML, Kopitas E. The effect of phacoemulsification on aqueous outflow facility. Ophthalmology 1997; 104: 1221–1227
Downloads
Published
Issue
Section
Categories
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
