Clinical Spectrum of Neuritis Optic Patients Receiving Intravenous Corticosteroid Treatments in Doctor Kariadi Hospital Semarang
DOI:
https://doi.org/10.35749/journal.v47i2.100303Keywords:
Optic neuritis, Corticosteroid, Visual OutcomeAbstract
Introduction and Objective: Optic neuritis is inflammation of the optic nerve leading to sudden loss of vision that takes place over several hours or days. Corticosteroids have been widely used in the treatment of optic neuritis due to their anti-inflammatory effects. This study aimed to retrospectively review cases of optic neuritis that have been the administration of intravenous corticosteroid treatment on visual acuity.
Methods: The authors conducted a retrospective study of patients who underwent 3 days of intravenous corticosteroid therapy for neuritis optic from January 2018 to December 2018 in Kariadi Hospital. The data collected included patient demographics, onset, clinical examinations, and visual acuity.
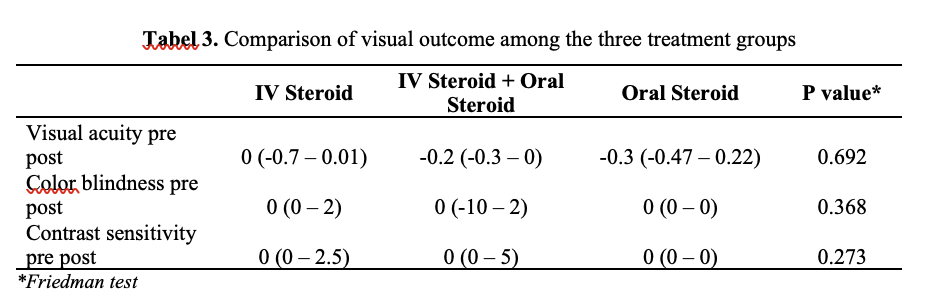
Result: The authors included 22 eyes from 16 patients who received intravenous corticosteroid treatment for 3 consecutive days during the study period. The study found a mean age of 32,91±9,32 years (18-49 years). The mean onset was 2,36±3,07 months (0,1-12 months). Ten eyes (45,5%) had positive RAPD and five eyes (22,7%) had ocular movement pain. Thirteen patients (59,1%) had papil edema in funduscopy examination. Fourteen eyes (63,6%) had visual acuity at or below 6/60 at the time of presentation. The mean visual acuity at the time of presentation was 2,45±1,79 LogMar units (Range 0,2-5,0 LogMar units). After three days of intravenous corticosteroid treatment, the mean visual acuity was 1,81±1,42 LogMar units (Range 0,1-5,0 LogMar units). The visual acuity before and after treatment were analyzed using the Wilcoxon test and gave p=0,004 as result.
Conclusion: Treatment of intravenous corticosteroid commonly gave a better visual acuity on neuritis optic patients. There are no significant differences of onset and clinical examinations in intravenous corticosteroid treatment visual outcome.
Downloads
References
Bennett JL. Optic Neuritis. Continuum (Minneap Minn). 2019 Oct;25(5):1236-1264. doi: 10.1212/CON.0000000000000768. PMID: 31584536; PMCID: PMC7395663.
Gal R, Vedula S, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database of Systematic Reviews. 2015;:2. doi: 10.1002/14651858.CD001430.pub4
Chan J. Optic nerve disorders. 2nd ed. New York [u.a.]: Springer; 2014. : 1-4
Mehrotra A, Saxena R, Jaffery N, Menon V. Comparative evaluation of megadose methylprednisolone with dexamethasone for treatment of primary typical optic neuritis. Indian Journal of Ophthalmology. 2007;55(5):355-359.
Singh D, Phuljheley S, Sharma R, Saxena R, Sharma P, Menon V. The Ophthalmology Open Journal. Clinical Spectrum of Pediatric Optic Neuritis in Indian Children. 2017;2(2):20-26.
Morrow SA, Fraser JA, Day C, et al. Effect of Treating Acute
Bioequivalent
Corticosteroids: A
Trial. JAMA Neurol. 2018;75(6):690–696. doi:10.1001/jamaneurol.2018.0024
intravenous
Optic Neuritis With Oral vs Intravenous Randomized Clinical
Miller DH, Thompson AJ, Morrissey SP, et al. High dose steroids in acute relapses of multiple sclerosis: MRI evidence for a possible mechanism of therapeutic effect. J Neurol Neurosurg Psychiatry. 1992;55(6):450-453
Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69(2): 292-302
Wilhelm H, Schabet M. The Diagnosis and Treatment of Optic Neuritis. Deutsches Aerzteblatt Online. 2015;.
Osborne B, Balcer L. Optic neuritis: Pathophysiology, clinical features, and diagnosis. 2018;.
PercyA,NobregaF,KurlandL.OpticNeuritis and Multiple Sclerosis. Archives of Ophthalmology. 1972;87(2):135.
Wang J, Tow S, Aung T, Lim S, Cullen J. The presentation, aetiology, management and outcome of optic neuritis in an Asian population. Clinical and Experimental Ophthalmology. 2001;29(5):312-315.
Saxena R, Phuljhele S, Menon V, Sharma P, Sinha A, Gadaginamath S. Clinical profile and short-term outcomes of optic neuritis patients in India. Indian Journal of Ophthalmology. 2014;62(3):265.
Volpe N. The Optic Neuritis Treatment Trial. Archives of Ophthalmology. 2008;126(7):996.
Chuenkongkaew W, Chirapapaisan N. Optic neuritis: characteristics and visual outcome. J Med Assoc Thai 2003; 86:238-43.
Singh D, Saxena R. Visual Outcome and Prognostic Factors of Optic Neuritis: A Perspective from the East. Delhi Journal of Ophthalmology. 2016;26(4):231-234.
DuY1,LiK,YangJ,XuX,LiJJ,ZhouRW, Zhang Y, Jiang BL, He JF. Disc swelling and mild initial visual acuity loss predict a better short-term visual acuity outcome in bilateral acute optic neuritis. J Clin Neurosci 2012; 19:1380-2.
Downloads
Published
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.